Vein Treatment
That Relieves Symptoms —
Not Just Appearance
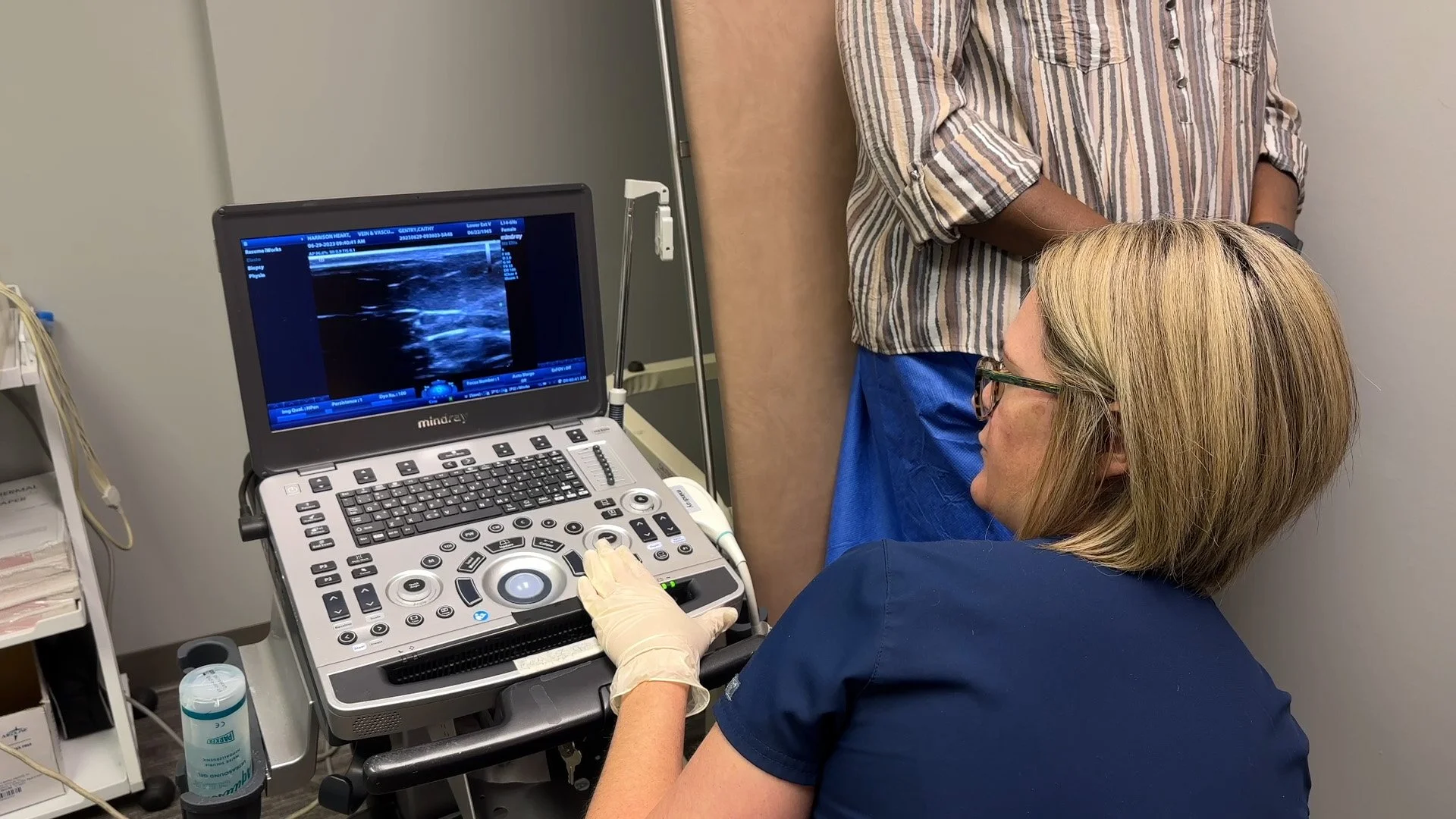
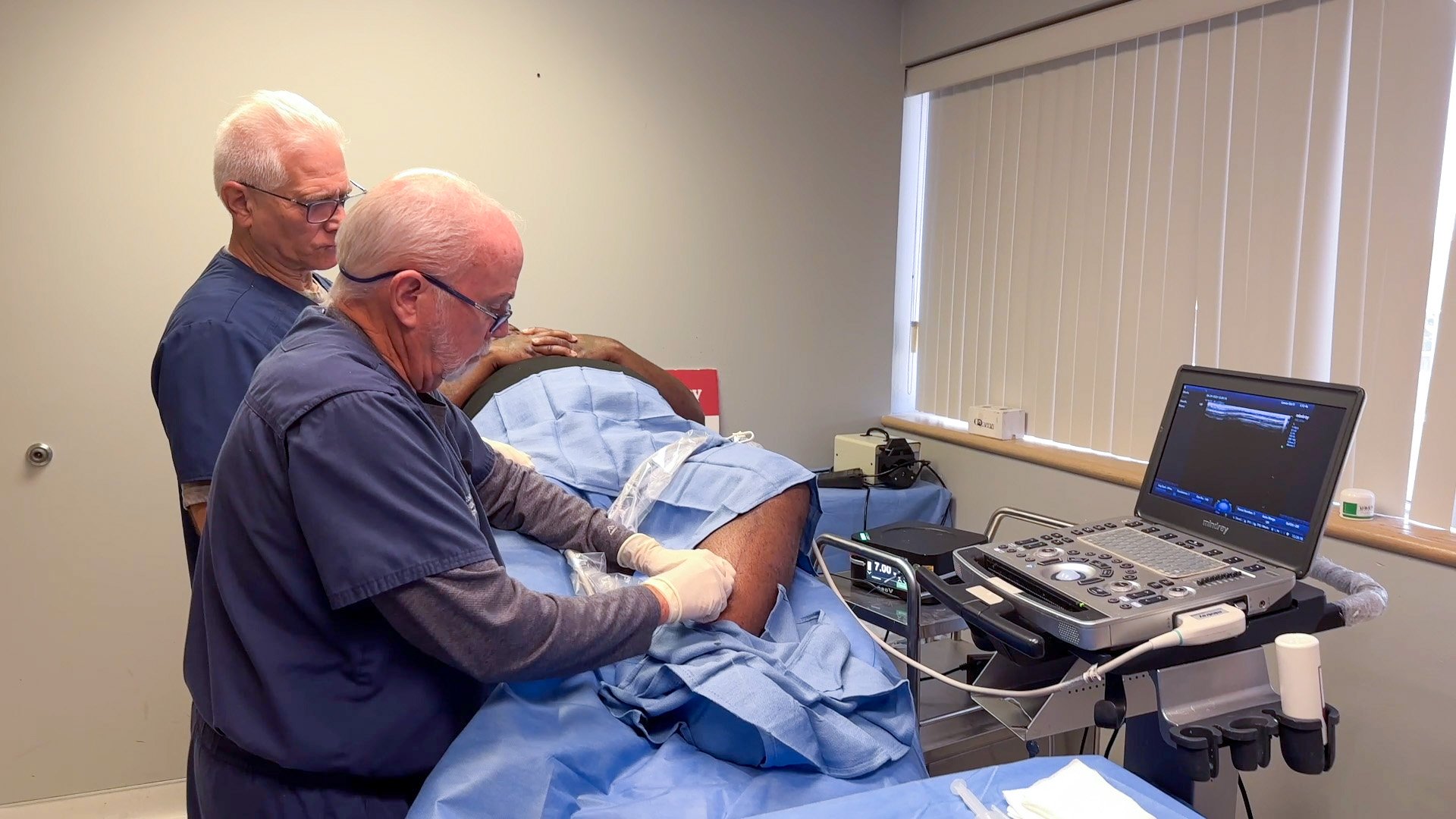
At Harrison Vein & Vascular, we treat the root cause of vein disease using modern, minimally invasive procedures—most performed right in our office.
If you’re dealing with leg pain, swelling, heaviness, or visible veins, effective treatment may be easier than you expect.
How Vein Disease Is Treated
Vein problems often start below the surface. When veins don’t circulate blood properly, pressure builds—leading to pain, swelling, and visible varicose or spider veins.
Our approach focuses on:
Identifying why symptoms are happening
Treating the problem vein, not just the appearance
Helping blood flow reroute naturally to healthy veins
✔ In-office procedures
✔ Little to no downtime
✔ Most treatments covered by insurance
Watch a Live Vein Treatment Procedure
Curious what it’s like to have a vein procedure? Watch this video to see an in-office vein treatment.
What to Expect at Your Appointment
Frequently Asked Questions about Vein Treatment
-
Most patients experience little to no discomfort. Local numbing is used, and procedures are well tolerated.
-
Most treatments take 30–60 minutes, depending on the veins treated and the technique used.
-
Many patients return to work and normal activities the same day or next day.
-
Yes. Medically necessary vein treatments are often covered, including Medicare. We verify benefits in advance.
-
The vein is closed and gradually absorbed by the body. Blood naturally reroutes through healthier veins.
-
Some patients notice improvement quickly, while others experience gradual relief over several weeks.
Expert Vein Care, Focused on Improving Lives
At Harrison Vein & Vascular, we specialize in diagnosing and treating vein conditions that affect comfort, mobility, and quality of life. Our clinic was founded with a simple goal: to provide patients with clear answers, effective treatment options, and compassionate care—close to home.
We focus exclusively on vein health, helping patients find relief from symptoms such as leg pain, swelling, heaviness, varicose veins, and spider veins using modern, minimally invasive treatments performed right in our office.
Physician-Led Vein Care You Can Trust
Our care is led by Lonnie Harrison, M.D., a vein specialist with decades of experience in vascular and cardiovascular medicine. While Dr. Harrison’s background includes advanced training in cardiology and endovascular intervention, his current focus is helping patients identify and treat vein disease early—before symptoms worsen.
Dr. Harrison has conducted vein screenings across Arkansas, educating patients about venous disease and expanding access to care. That same commitment continues in our clinic today, where every patient receives thoughtful, individualized attention.